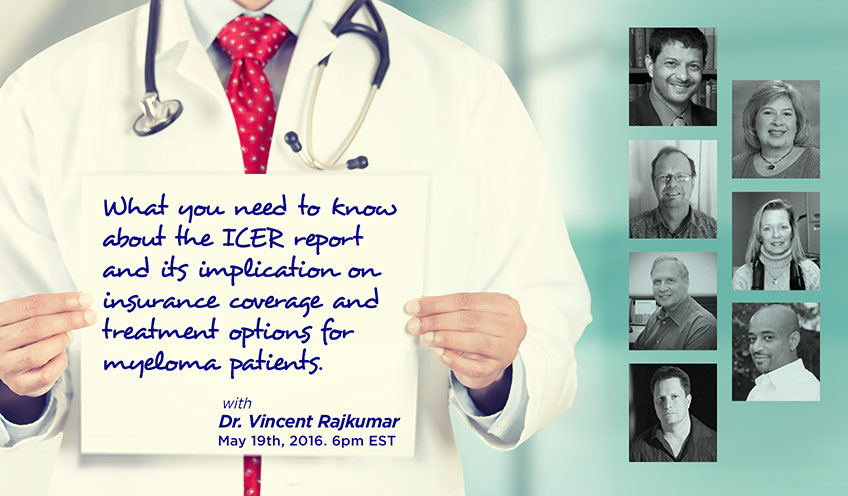
Priya Menon – Good evening and welcome to CureTalks. I am Priya Menon, Scientific Media Editor of CureTalks, joining you from India. This is CureTalks’ 105th episode; and today, we are talking about multiple myeloma. On the myeloma panel today, we have eminent patient experts and myeloma advocates, Jack Aiello, Cynthia Chmielewski, Nick Van Dyk, Yelak Biru, and Lori Puente. My co-host for the evening is Gary Petersen, editor of myelomasurvival.com. Welcome to CureTalks.
Priya Menon – Cancer drugs cost more than 100,000 dollars per year and continue to increase. Medicare has proposed major changes to Medicare part B in an attempt to slow the explosion in healthcare expenditure. In addition, a recent report by a group called ICER, Institute for Clinical and Economic Review, has issued a 179-page draft of a report, attempting to evaluate multiple myeloma, its treatment protocols, drug cost comparisons, and quality adjusted life year. The results of ICER’s research may have serious implications as their recommendations are trusted and used by payers and maybe influencing CMS decision making. Dr. Vincent Rajkumar of Mayo Clinic is on CureTalks to help educate doctors, patients, and the general public on what these programs are and how they might affect the doctor-patient relationship. Dr. Rajkumar is a Professor of Medicine at the Mayo Clinic in Rochester. Welcome to CureTalks, Dr. Rajkumar. Its a pleasure to have you with us again.
Dr. Vincent Rajkumar – Thanks, Priya. Thanks for having me.
Priya Menon – Before I hand over to Gary to begin with the discussion on a very important topic, I would like to remind our listeners that we will be addressing questions sent in via email towards the end of the discussion. If you have a question for Dr. Rajkumar pertaining to the topic under discussion, please press 1 on your keypad and let us know or mail it to priya@trialx.com. You can also post it on our website, curetalks.com. With that, its over to Gary. Gary, you are on air.
Gary Petersen – Thank you very much, Priya, and…, and thank you so much for bringing this forum for us so that we can discuss very, very important topics, not only important to myeloma patients but cancer patients in general and this happens to be one of those topics. Not only is Dr. Rajkumar the Professor of Medicine at Mayo Clinic, but if I went through his curriculum vitae, it would take most of the hour, so I won’t do that. I’ll just leave it at the fact that I consider him to be a part of the Mayo Clinic dream team and… and…, in fact one of the great eight myeloma specialists in the world; and I’d say that most people would consider him in the top 10 of all myeloma specialists who would look at his excellent history of…, of works. Not only is he a great doctor, but he is a patient activist who has taken on a major issue of runaway drug costs for cancer therapy. We are number 1 in spending in healthcare, significantly greater than the second, which is Norway and being number 1 in healthcare, you would think that we would have some great healthcare outcomes, but we are 33rd healthiest nation in the world, just one ahead of Bosnia which is one of the poorest countries in Europe. He has taken leadership role in bringing this issue front and center and doing it in the face of hurricane winds of special interests, you know, and lobbyist influences and conflicts of interests. So, Dr. Rajkumar, welcome and thank you so much for all of your efforts and…
Dr. Vincent Rajkumar – Thanks, Gary.
Gary Petersen- Thank you so much for bringing this fight front and center and taking on what I consider monopolistic pricing with regard to cancer drugs. You and 118 cancer experts have made some excellent recommendations in Mayo proceedings and can you explain the proposed Medicare part changes and also the ICER report and…, and what is your read on the value and quality of these efforts, you know, given the backdrop of your own pretty in-depth evaluation of rising costs of healthcare in this nation?
Dr. Vincent Rajkumar – So, Gary, first of all, thanks to you and Priya for having me on CureTalks. This is a very, very important topic; and I am glad that I am able to spend some time addressing this. Now, in order to understand the Medicare part B changes and what ICER’s report contains, one has to understand the background really, really well because much of this is unique to the United States. First, the facts… The facts are that almost every new cancer drug is priced at more than 100,000 dollars a year, whereas the median income in the United States is around 50,000 dollars a year. There are also co-pays of 10% to 20% that are added on to new drugs; and while the well insured may be able to get away with policies that don’t have co-pays, the under insured and uninsured are the ones taking the brunt, particularly middle class who are not a…, not poor enough to get assistance and not wealthy enough to have the greatest of the insurance policies. There is also no relationship between the value a drug provides and the cost. So, a drug that prolongs life by one month is priced at the same range as something that would prolong life by a year or more. Question then is why are cancer drugs so expensive in the United States and…, and in many other parts of the developed world. I mean the easiest answer is…, it costs a lot of money to develop a new cancer drug and that cost has to be recouped, not every drug that is developed is successful and therefore, you also have to add on the costs of all those failures when you finally have a success.
Dr. Vincent Rajkumar – There is…, but there are other important reasons why the…, why drugs are so expensive that we should get into. If you take any other product that is marketed, there is usually a competitor and having three or four different phones is why you have the iPhone at a reasonable price. The lack of a generic price check having four different versions of carfilzomib or four different versions of bortezomib means a company has virtually a monopolistic control over that particular drug and the lack of a generic price check is really critically important and when you…, when you wonder why the costs are so high and then the seriousness of the disease. I am just like any of you. If one of my family members has a cancer, whether the drug prolongs life by a week or two weeks and no matter what it costs, I am going to try and get it, even if it means mortgaging my house or selling property. So, the seriousness of the disease means that we are willing to pay no matter what the price is.
Gary Petersen- Your money or your life.
Dr. Vincent Rajkumar – …and then there is… Yes, and then there is the…, there is the incentive to prescribe more expensive chemo based on the way we reimburse chemotherapy in the US. In private practice, oncologists are reimbursed a proportion of the average sales price of the drug. So, if you can choose between a drug that costs 1,000 dollars and 5,000 dollars, the average take home that you can make would be more with the more expensive drug and that I am not saying oncologists do that, but there is an incentive to prescribe more chemo and more expensive chemo and…, and…, and like I said, there is no market forces that play. Usually, in a free market, a buyer and seller negotiate price. You have a variety of things you can choose from; and you have the opportunity to walk away from a bad deal, none of which apply in this…, in this area. So, there is a monopoly and even if you have five drugs to treat a particular disease, there is still a monopoly because in a disease like myeloma, nobody is going to say that we’ll just try two drugs and stop. You are going to try every drug; and if you are going to try every drug, then each drug is…, is virtually a monopoly.
Dr. Vincent Rajkumar – Let me get into what can we do about this. How can we…, how can we reduce the cost? Most developed countries, approval of a drug is only the first step. The second step is a regulatory authority, usually a governmental agency, will negotiate with the seller, pharmaceutical companies, the price of the drug that’s based on the value it provides. We do not have a mechanism like that. We do have an institute that was set up called PCORI. This is supposed to look at cost effectiveness research, but supposed to look at competitive effectiveness research but is prevented by law from looking at cost. Now, we are not able to import drugs from other countries where the same drug might be available for cheaper prices and allowing PCORI to look at cost. Having an agency after the FDA approval to look at cost and the value the drug provides in order to get the drug approved and on the market and allowing importation of drugs will all go a long way into reducing the cost, but we need more than that. I think couple of things that we really need are allowing more free entry for generics, allowing the biggest buyer of drugs to negotiate prices, that is Medicare, which is now restricted by law from negotiating prices. Therefore, the only thing Medicare can do is to tweak the regulations and that’s what part B changes are all about; and some of your questions later on are in more depth about that and so I will go through what are the specific part B changes when I come to those questions.
Dr. Vincent Rajkumar – And finally, agencies that can look at value and that’s where the Institute for Clinical and Economic Review comes in. This is a non-profit organization that basically assists the evidence that we have currently and makes cost-effective recommendations. How can we accomplish these goals, these big sweeping changes in post-drug…, post-drug approval review or allowing importation or allowing Medicare to negotiate prices. These are not easy to do and we need allies that can lobby Congress and lobby the people in power to make these changes; and unfortunately, if you look at the situation, there are very few allies in this fight, mostly patient organizations, professional organizations, and these patients are being silent in terms of going and asking for lower prices because of various reasons. I think we need to come together to try and see if we can address the rising costs because year after year the costs are going up and at some point its going to be unsustainable.
Gary Petersen- Okay. Now, that was A and D and…, and ICER, you talked about, both of those things. One of the things that I noticed with regard to ICER is ICER is much like NICE, which is the program that they have in the UK and what that does is it…, it goes through and comes up with an economic model for whether or not to approve drugs or…, or not based on their cost effectiveness, but, you know, because they can, in fact, negotiate price and they do so to the extent that I think they halved the price. The cancer drugs in Europe are half or they are here that, you know, when they go through one of these models effectively, you know, their…, their cost is half as much, so they are twice as likely to not consider one to be cost effective than if you would be in this country where you don’t have any controls or any negotiating price. So, I thought, you know, that was…, that’s something that makes ICER a little bit different here. The other…, the other thing I wanted to ask was the ICER report, in my opinion, you know, seems to be flawed and has been likened to what NICE is, which is the same kind of program but its for that which is in the UK and they have nationalized healthcare and they use it to allocate their scarce medical resources and what I mean by that is we do not have national healthcare here and we spend twice as much on our healthcare and because of that one would expect, you know, that we would be able to, you know, obtain much better care with that. Unfortunately, that’s not the case, but the fear is that this is our system and if you overlay, you know, a mechanism for nationalized healthcare on top of that, you know, will that in effect limit doctor’s treatment options and put it in the hands of the insurance company policy and not in the hands of the doctor’s and so that’s my fear and you will see that its a…, the fear of many of the people on the panel as they discuss this. What are your thoughts with regard that?
Dr. Vincent Rajkumar – Okay. That was very…, that’s very important. I think I need to address the two…, the two concerns you made. Just tongue in cheek, I would just say NICE is just a place in France. You know, there’s a vague book that you can go and check out. I think first of all, people need to understand what NICE is if you have to distinguish it from ICER. NICE is a governmental agency in the UK. Its the National Institute for Health and Care Excellence. It is charged with looking at the drug pricing, and the system there is that the government pays for the drugs. So, the government has only a limited amount of budget and with that it has to pay for all of healthcare. So, if a drug company suddenly comes in and says, my drug costs 200,000 dollars a year and all patients should get it, someone else has to have cuts. So, NICE evaluates all new drug approvals to decide what is and what is not cost effective and what they can afford and if the manufacturer prices the drug so high, then they walk away. So, really if they didn’t have NICE, then they will go broke because, you know, they have a very limited budget to pay for all drugs. I mean, if the government is paying for it, they do have the right to negotiate the price with the seller.
Dr. Vincent Rajkumar – NICE is not unique though. All European countries have a secondary review mechanism where a drug approval simply gets the drug approved, but in order for reimbursement to occur, another agency like the Health Authority in France will then negotiate with the pharmaceutical company about what the price should be; and this is based on the fact that there are no infinite resources, not in the UK, not in Europe, not in the United States either. There is only a finite part; and if you take a lot of money from that, someone else is going to get hurt. So, for example, the median income in India is 1,500 dollars per year. Its simply not possible for a drug that costs 100,000 or…, or a regimen that costs 300,000 dollars to be used. In the UK, the median income is 32,000 dollars. So, they have to work within those limits to see what’s affordable. For example, carfilzomib-lenalidomide-dex that is the…, was done…, was a study that I led and…, and was published in the New England Journal of Medicine. That regimen works and first relapse for 27 months for a cost 420,000 dollars in the US and you have to take that into account. So, agencies like NICE and Health Authority are needed if countries are to survive with their healthcare budgets.
Dr. Vincent Rajkumar – ICER, on the other hand, is not government. ICER is just like you and…, you…, you and me forming an organization. They are a non-profit organization. They get funding from various sources, including non-profit foundations, and they basically look at the evidence that’s out there and put out a statement. Unlike NICE, they don’t have regulatory authority and the only reason somebody will listen to ICER is if they find them credible. The…, the less credible they are, insurance companies are not going to go there or neither…, neither are patients going to be willing to accept what they say and just like ASH cannot tell ASCO what to do, I don’t think anyone can regulate what organizations in the US that are non-profit, if they wish to put out a report, yes or no, but we can comment on those reports. We can give them input. With ICER, at least I think what you have is the many steps here involve, the first is the putting together an evidence packet. That is the 179-page report that Priya mentioned, which is just basically a summary of all the evidence that’s out there and then their own interpretation of how it will cost based on the market value of these drugs to give these regimens.
Dr. Vincent Rajkumar – Then, you have input from patients, physicians, the general public to a panel of non-conflicted, non-myeloma experts who are well versed in the economics to decide, you know, what the questions are and what the questions to be answered. A lot of the concern with ICER has come based on the report but on the answers to the questions because the questions haven’t been answered yet and it looks like everybody’s concern is based on how they think the questions will be answered rather than, you know, wait. I think the anxiety over ICER is pretty premature and I think when the…, when the answer is going to come out, then its the time to…, to see whether that…, the right call was made or not and those answers and comments are going to be with the input of experts, patients, public as well as all the people who have already provided opinions, but just remember that without pathways based on cost effectiveness where someone is willing to say that this particular regimen that you are charging 500,000 dollars is just too much and not worth it, there will be no reason for companies to lower cost.
Gary Petersen- I hear what you’re saying. I…, I looked at that report and they just put on the…, you know, they just put on the executive summary on the top of that and what it…, what it tells me is that no drug, either of the drugs that are there for second and third line approval is cost effective. So, you know, what it suggests to me, you know, and I think anybody who would rate it is that…, is that if…, if somebody looks at that they might want to use that as evidence that everybody should get lenalidomide and dexamethasone for second and third line and that’s it, but…
Dr. Vincent Rajkumar – I don’t think that the odds are…
Gary Petersen- That’s…, that’s how I read it. You know, from the executive summary.
Dr. Vincent Rajkumar – I…, I don’t think you need to worry about that and I will address some of those things later.
Gary Petersen- Okay. Well, I am…, I am glad you are there to add some logic to the whole thing because I think that there are some major holes in it, you know, I am not against what they are doing. I am just against the assumptions that are used in the analysis and I am also against, you know, in my own opinion and using something that should be used for national healthcare in a…, in a…, in a…, you know, in…, in insurance-based industry, but I also believe that, you know, its something that we can do something with if we had any politicians that really were looking at the public interest and treated the monopoly like a monopoly, but given that, that’s my opinion and Jack has an opinion as well. Jack, are you online?
Jack Aiello- Yeah, I am. First of all, Dr. Rajkumar, thanks so much for being part of this. I…, I don’t say I hate seeing you spend time on this. I’d much rather you be focused on more clinical trials and.., and (laughter) doing the things you do for myeloma patients, but I appreciate this. I…, actually someone told me that the ICER report was funded by…, 70% by Houston billionaire named John Arnold and the rest of it by, 30% by insurance companies, company-funded foundations. So, they may be non-profits, but I think there is strong insurance backing behind that. My concern as I read through the report and I had this with the report as well is that no matter what numbers you fiddle around with, it still comes down to the high cost of drugs which the ICER report really doesn’t do anything to control cost of drugs. It just reports on the high cost of drugs and that’s used in different ways and the biggest concern, I think that Gary alluded to it, is if this report is accepted, will insurance companies use this information to limit treatment to patients and if so what can we do about it?
Dr. Vincent Rajkumar – Okay. Jack, first of all, like I have…, I have…, many times I have wondered whether, you know, if this is something I should just give up on, but myself, Hagop, and others, we feel like, you know, that when we see patients suffer or when we actually look at what the future will hold where this kind of rising cost is just unsustainable, that eventually patients won’t have access to the important drugs because you don’t have the money. I feel like this is something we have to continue to…, to highlight. I…, I do understand your concerns and I think…, let me just, you know, let me just go through like, you know, what your concerns are and then point out where the flaws are.
Dr. Vincent Rajkumar – Number 1, you know, the fact that many of these new regimens, carfilzomib-len-dex, ixazomib-len-dex, or…, or, elotuzumab-len-dex cost so…, so much, you know, 200,000 to 300,000 dollars, is not the fault of ICER. This…, this is the reality. These medications are very expensive and when its put out there and says that, you know, this regimen increases life by one year and…, and taking this regimen for two years is going to cost you so much money. Nobody is putting a value on life. What people are saying is this is what pharmaceutical companies are charging for you. It is not ICER or me or anyone else putting the value on life, this is what…., and then the question is what are other countries paying for an extra year of life and if you look at… I am…, I am going to talk about QALYs later because some people have had them. The general…, general extra year of life what other countries are willing to pay for is…, is much, much lower than we currently do and there is an amount that economically is feasible based on the per capita income of a country, what is really feasible. Like in the US, the maximum feasible per extra year of life to be having a sustainable country would be like a 150,000 dollars. That doesn’t mean that’s what we put on the value on life, that’s what generally the price of drugs should be or price of regimens should be and we are far away from that now. You also have the problem here that the facts are not that new drug costs so high, its also that old drugs cost high.
Jack Aiello- Yeah.
Dr. Vincent Rajkumar – The drug prices that you saw with Turing Pharmaceuticals where the price went from 13 dollars 50 cents to 750 dollars overnight with Daraprim. That’s not an outlier. That’s an outlier only because it happened overnight. Many, many drugs… Many, many cancer drugs, the price continues to increase year after year, which you would think is completely unreasonable since the development cost was already taken care of. Gleevec, for example, cost 21,000 dollars per year in 2001 and a 132,000 dollars per year in 2014. Thalidomide cost a 168 dollars per month before it became a myeloma drug, then it became a few thousand, now its 4,600 dollars a month. Melphalan, doxycycline, you take any drug, the prices continue to increase because this is not a free market system. There is… The person paying the bill unfortunately, the vast portion of the bill is a third party. Its either government for all Medicare patients or the insurance company and the buyer and seller cannot negotiate. So, these are the reasons why the costs are high and what ICER is trying to do is give you… These are five options for physicians to use, just here are the costs that will go with each one of these and the questions asked are – Is there data to show that any of this is better than standard and you don’t know the answer to that because that will be decided only by the panel in the future. All these worries are coming from people who think they know how the question is going to be answered.
Jack Aiello- So, you don’t think insurance is going to necessarily adopt a stance where it says we will approve this one and…., and make it something analogous to a tier 3 payment payout versus if you choose a different one, we are going to make it a more expensive tier 5 payout?
Dr. Vincent Rajkumar – You know, I am not part of ICER. I am just one of the people who will be at the…, at the…, at the meeting, but I…, I really have not historically found that this is going to happen. Remember, insurance companies do not need ICER to decide what they will and will not reimburse. Insurance companies today can say, we will reimburse according to the label and that label then would restrict you far more because they also have to be sustainable, right? You cannot… The problem with…, with myeloma is that the cost of treating a myeloma patient over one year had just doubled overnight with approval of three new drugs. So, then what happens is, insurance companies have to adjust their premiums for everyone else to make themselves just stay afloat. They can do that or they may just decide that we will put restrictive practices. They really don’t need ICER’s help or ICER’s endorsement to change the way they reimburse or allow. They can just say, we will reimburse according to the FDA label, which is what we are allowed to do and then you have the situation where none of these regimens which were all developed in Europe and other countries where patients never got lenalidomide and dex, when we want to use…
Dr. Vincent Rajkumar – When I go to my clinic, I have a patient who is already progressing on lenalidomide and dex and I am not going to choose either carfilzomib-len-dex or ixazomib-len-dex or elo-len-dex. I might use, you know, pomalidomide plus carfilzomib-len-dex. What if the insurance company says, we will not reimburse that? That is not even part of the ICER report or that doesn’t even go there. I am trying to tell you that insurance companies can do that today without the help of ICER, but in general, they have been very good about allowing wide freedom to clinicians to do what we want to do because of various justifications we make, you know, in terms of patient’s health, life, safety, and we are going to be advocates for you, but I think the…, the…, the reason this will collapse would be due to unsustainable prices. If KRd costs 300,000 a year and tomorrow everybody wants to use daratumumab plus KRd and it costs 400,000 dollars a year, that’s when the insurance company might say label, otherwise I am not reimbursing. So, we have to go to the pharmaceutical companies and ask them why are we not…, why are we charging so much.
Jack Aiello- Yeah, and my second question really has to do with the drug costs and really they are market driven more than anything else, Gleevec being a perfect example that you noted earlier, and I wonder from a physician’s viewpoint, are there more cons or pros if…, if we ever considered going to a…, a single payer system such as Medicare able to negotiate costs and could it fix this or would it put more handcuffs on research and such?
Dr. Vincent Rajkumar – No, I think, You know, honestly, I was at the healthcare forum and the head of Kaiser Permanente just laid out a great example. He said like, listen, I have a multi-billion dollar industry, healthcare industry. I negotiate with people all the time and we…, someone asks me like, I will sell you this for 200,000 and we reach…, we reach a deal. The problem with healthcare is if companies says, this drug costs 150,000, there is no bargaining power because they could walk away and what you cannot say that I won’t give this drug to my…, to my patients. Medicare is the biggest buyer. It spends over, you know, I think 150 billion or something like that on prescription medicines and Medicare cannot negotiate by law for…
Jack Aiello- Right.
Dr. Vincent Rajkumar – …over prices of drugs. If that was written into the law when part D was passed, it basically gave a huge benefit to the US population which said that all Medicare patients who are enrolled in part D will now have prescription drugs covered, but it also said that Medicare will buy the drug from companies for whatever price they name and that’s what led to all these runaway prices. Even then people predicted, like Dean Baker, that this would cost Medicare 600 billion compared to if they were able to negotiate. So, I really think that Medicare being able to negotiate directly with pharmaceutical companies on how much they will buy the drugs for, which they are currently prevented from doing, will have…, will go a long way in controlling prices and that does mean temporarily patients have to be willing to accept the fact that Medicare will have the power to walk away from a bad deal, like they might say like, this is too high, we cannot afford it, which is what other countries do, but, you know, I think one thing that most people don’t recognize is that the US acts as a safety valve because Medicare cannot negotiate and the company then can more forcefully negotiate with just about every other country because if UK says we will not…, we cannot afford this drug, they can…, the company can simply walk away and say that whatever loss or profit in the UK, they can always make it up in the US. We act as a safety valve.
Gary Petersen- That’s…
Dr. Vincent Rajkumar – There is really no feeling on the prices here. If we can negotiate, that will, I think, help everyone because then the power of being able to walk away is what will lower prices.
Jack Aiello- Thanks very much, doctor. Gary!
Gary Petersen- Yeah, Jack. Thank you very much. Cindy!
Cynthia Chemlewiski – Hi!
Gary Petersen- Your questions.
Cynthia Chemlewiski – Can you hear me now? I am on. I am on.
Dr. Vincent Rajkumar – Yup.
Gary Petersen- Yes, you are on.
Cynthia Chemlewiski – Okay. Thanks, Dr. Rajkumar, for enlightening us on all these areas and my mind is kind of spinning over here because I am pulled in both directions. I agree that we need to somehow find a way to lower the prices because they are skyrocketing and some people just cannot afford it, no matter what kinds of supplements they are given and it scares me at the same time because I don’t know if its going to limit my access. So, I am just…, I am going to focus in on the proposed changes to Medicare part D, not the negotiation but the way that reimbursement is and I…, I think I am understanding that currently you were saying that drugs are reimbursed. The person who prescribes them gets 6% of the cost of the drug and ….others will now get 2.5% cost of drug plus a flat fee of, I was reading like, 16 dollars and 80 cents. Do I understand it correctly, is that correct?
Dr. Vincent Rajkumar – Yup.
Cynthia Chemlewiski – Okay. So, at first that sounded pretty cool to me, I was okay. This may be a good idea because this way people …to gaining an incentive to prescribe a higher-priced drug, but then I started reading things written by ASCO and they were concerned about Medicare part B changes and they were asking them to withdraw these changes and I guess what they were saying was that they did some type of modeling of proposed formula and when they modeled it, they used some like 28 practices representing 425 oncologists in 25 states and they showed that an office of about 15 physicians would lose about 560,000 dollars a year and what their concern was if they are losing this much money out of their operating budget, they are going to have to make some cuts and they were concerned that the cuts must not be made in the doctor’s salaries, but the cuts may be made like reduction in staff such as nurses, patient navigators, and social workers. So, what is your take on that?
Dr. Vincent Rajkumar – Oh, thanks, Cindy. Thanks for wanting me to discuss the part B changes. So, just for people to be aware, the one that we talked before is part D as in “David” that deals with prescription drugs that Medicare is prevented from negotiating the prices for.
Cynthia Chemlewiski – Okay.
Dr. Vincent Rajkumar – Part B is for drug, the one that I am going to talk about now, part B, is based…, is for drugs that are intravenous or subcutaneous or some other parenteral form that is administered in a doctor’s office. So, you just need to know what the current model is. Many, many oncology and chemotherapy drugs, some of the most expensive drugs are administered in doctor’s offices. Doctors actually buy and then administer the drug. In essence, they function like pharmacies. They buy the drug, they administer the drug, and they charge Medicare for how much ever it cost for them to get the drug. What Medicare does right now, it reimburses physicians, whatever the average sales price of the drug is, plus 6%. So… And that then means that if you have two drugs, one is 1,000 dollars and one is 10,000 dollars, you will get far more money dispensing the 10,000-dollar drug in terms of profit because he gets 6% of that and this you can look at Taxol versus Abraxane or many, many similar drugs which bortezomib versus carfilzomib. There is a built-in incentive to use the more expensive drug which has the better reimbursement, 6% of that is…, is…, is actual profit. Now, of course, if they buy the drug for a much more higher price, then they don’t make that margin, but…, and generally would assume that all things being equal the universe of oncologists every drug, the average sales price plus 6% means pretty much most people are making 6% of what they overall sell.
Cynthia Chemlewiski – Okay.
Dr. Vincent Rajkumar – …and that is then giving an incentive to give more expensive chemo and this has been shown in studies that doctors generally don’t give chemo to a patient who doesn’t need chemo just to make a profit, but there is a study that has shown that in general if…, if two…, two drugs are equal, they would choose the more expensive drug. Now, what does Medicare… What does Medicare do? Medicare’s proposed changes are that instead of giving 6% of average sales price, which is quite a bit for considering oncology drugs are so expensive, they said we will give 2.5% over and above the sales price. So, you buy the drug for 1,000 dollars, we will give you 2.5% of that over…, over and above that 1,000 dollars plus 16 dollars and 80 cents. Now, that 16 dollars and 80 cents is interesting because what it does is, a drug that costs less than 500 dollars per day to give, the oncologist or practitioner will now make more money with this system than…, than before, but… So, it really affects only drugs that are very highly priced…
Cynthia Chemlewiski – Okay.
Dr. Vincent Rajkumar – …and that is the first proposal. The second proposal is that they will eliminate the co-pays for patients. So, if you have to pay 20% of your bortezomib or carfilzomib, they…, they will eliminate that. So, you won’t have out of pocket. The third change is that indication-based pricing, that means a drug is approved, let’s say, for myeloma and it prolongs survival by one year, so legitimately the company charges 100,000 per year. Let’s say I use that same drug for some other cancer for which it works only for one week. They will not give me the same dollar amount because this is a completely new indication for which the benefit is very, very low. So, its more indication-based pricing. And then the fourth big change was reference pricing. If there are three drugs that are fairly equal, similar mechanism of action, similar drugs, then they will reimburse one fixed price regardless of which drug you choose and that then eliminates the…, this desire to give the most expensive variant. These, I think, are very common sense proposals; and I am actually flabbergasted at why so many organizations are opposed to it and some of them came out with an opposition within one or two hours of the Medicare part B and I am a member of many of these organizations, I never heard of them, nobody ever talked to me or got our feedback, but its important to recognize why Medicare is doing it.
Dr. Vincent Rajkumar – Medicare spent 140 billion dollars on prescription drugs in 2014. Every year the price of how much Medicare spends to provide healthcare keeps going up. It went…, it goes up 6% or so for all of healthcare, but it went up 14% for prescription drugs. That means the fastest rising cost in Medicare is prescription drugs. Again, this is a real sum game. There is only so much money in Medicare. If drug costs go up and keep going up and take up a larger and larger fraction of Medicare spending, the reimbursement that Medicare gives for all other services has to go down. That is why patients will slowly find it harder to harder to get into doctor’s offices, hospitals because people are saying we don’t want to take Medicare patients as Medicare reimbursement goes down. So, there is a price to pay. If Medicare pays more for drugs, there is less for other things and that means cutting off access to other…, other, you know, already people are saying that its very hard to get the Medi and myeloma is a disease of elderly people.
Cynthia Chemlewiski – Right.
Dr. Vincent Rajkumar – Now, ASCO is concerned that, you know, there is a huge, you know, for a 15-physician practice with 560,000 dollars in loss would occur, but I…, I…, I…, I find that hard to believe. Even if that is true, that’s only 30,000 dollars per year per person and the last time I checked the oncologists are some of the best paid doctors in the country and doctors are generally in the top 1% of progression or so. I mean I think we’ll have to take all of this with…, with…, with advice. I would be very happy if the degree of pushback I have seen with regard to ICER and Medicare part B from various professional organizations and patient organization were directed at pharmaceutical companies to lower cost.
Cynthia Chemlewiski – Okay. That kind of makes sense. It just…, you know, I got concerned when I saw a big organization like ASCO not wanting to support these kinds of changes and this kind of gets everything in my mind as to why this might be the case. I…, I guess the other thing that ASCO was saying and maybe you comment on it too, is if these part B changes do occur, they believe that more drugs will become underwater drugs and I am not quite sure what that means, an underwater drug, if you could explain that, but it… My take on it was that these drugs would be too expensive for an oncologist to access the pharmacy to buy the drug and to administer it, so that the local oncologist can…, may prescribe the drug but instead of getting the drug right there in my oncologist’s office, I may have to go to a cancer center to get that drug. Is that what ASCO was trying to say or did I get that whole thing wrong?
Dr. Vincent Rajkumar – No, you’re right. So, under-water drug means that if a…, if a physician purchases a drug for higher price than what Medicare is reimbursing, then that would mean that they are losing money every time they give that drug, but, you know, you have to look at the Math here, I mean the law for averages. For every drug that they purchase at…, at a cost higher than what Medicare reimburses, there will be many drugs that they purchase at a cost much lower than what Medicare is reimbursing. So, it will all be a wash. So, I am not sure that this is such a major concern. Second thing is Medicare is doing this as an experiment. Its randomizing the whole country by zip codes and…, and just basically half the country will have the changes, half won’t and they will look at it year after ye2ar to see whether what they are doing makes sense and whether it actually saves costs or causes problems. So, this is a good experiment. Its not something that we can decide how it will turn out before we even do the experiment.
Cynthia Chemlewiski – So, this is kind of an experiment, we are going to see what happens…
Dr. Vincent Rajkumar – Yeah.
Cynthia Chemlewiski – …before they do the…
Dr. Vincent Rajkumar – Yup.
Cynthia Chemlewiski – ….and how are they going to randomize, just pick it up….
Dr. Vincent Rajkumar – By zip codes.
Cynthia Chemlewiski – By zip code?
Dr. Vincent Rajkumar – By zip codes.
Cynthia Chemlewiski – Okay.
Gary Petersen- Yeah and I think, doctor, one of the things that we see is that…, yeah, this affects the doctor and whereas ICER affects…, could affect the patient and so as a result, you know, we are kind of more interested in the ICER part than we are in the A and B, or the error of the B part and because it affects more how the doctor is being reimbursed and if it drives cost down, we’re all for that, but obviously some people, and its the doctors, some of them don’t like it. Cindy! I think we need to move on, is that okay?
Cynthia Chemlewiski – Okay.
Gary Petersen- All right. Thank you. Nick, you online?
Nick Van Dyk – Hi, folks! So, I think we have all heard that there are no atheists in the foxhole and there are probably not a lot of people in favor of things that reduce their drug options if they are reliant upon those drugs to live. So, first, I applaud the good doctor in engaging with a group of people that could be prone to be a little panicky over this stuff. (Laughter) So, insurance companies can do what they like without ICER, of course, but a report like this does give them a lot of ammunition and a lot of analysis that they are probably ill equipped to undertake and puts it all in one place for them with a bow on it and the power to walk away, of course, can lower prices as can the availability of generics, but Celgene can’t be forced after all to develop a successor to pomalidomide and the day that it becomes less profitable to develop personalized immunotherapy for 100,000 people than it does to make a cheaper, improved version of Viagra, big pharma is going to start spending more money on marital AIDS and less money on cancer. May be at the limits of 100,000 per year, that gives us some headroom, but in the meantime, there are lot of big issues that will have to get solved, so I am thankful that you and others in the private and public sector are working on them, but we are still sort of stuck in between at the moment. So, as of where we are right now, I would be interested in knowing why ICER picked myeloma. Is it really just a polemic against pharmaceuticals or is there a…, is a…, is there a particular patient advocacy goal here and in an environment where we don’t have enough data really about the long-term success of a lot of these novel therapies. Is it even the right time to issue such a report?
Dr. Vincent Rajkumar – Nick, as usual, you always have fantastic questions; and I think this is a great question. Why did I choose myeloma. I don’t know, but if I were to guess…, myeloma has become one of the most expensive cancers to treat. One year of bortezomib-len-dex can be 200,000 dollars a year. One year, if someone decides…, some oncologist somewhere decides that I do not want to use bortezomib-len-dex, I will just use carfilzomib-len-dex and sit for all my frontline, they just increase the cost of myeloma therapy to 300,000 dollars per year. So, ignoring ICER for a second, you have to ask yourself should there be some guidelines to suggest what would be the best frontline therapy as…, as far as data goes and can someone really on their own change the cost of care, an extra 100,000 per patient and say that that’s their standard of care and this is going to be bigger and bigger problems because somebody may want to give daratumumab on top of this and change.
Dr. Vincent Rajkumar – So, in my experience, insurance companies would rather have a predictability in how much it costs to treat myeloma and so if in southern Minnesota it costs 100,000 dollars per year and Minneapolis it costs 200,000, that’s what causes the problem. The problem is variations across regions, variations across doctors, for no reason, no…, doesn’t seem to be any particular different types of patients that they are seeing and so what ICER is doing here is to just provide the data and like I said, I know that people are panicked just because they saw the dollar amount attached to what it costs to give an extra year of life in relapsed setting and first relapse and second relapse, but I think you want to focus on the seven or eight questions that were in the panel thing because that’s what you want to ultimately see, like, you know, how are those questions answered and not worry about the background information, which is extraordinarily dense, like, you know, very detailed and that is just the data. It is raw data without making a… It just is jarring because when you see that that’s how much it costs and bear in mind that this may even be an overestimate, you know, in terms of like…. It may even cost much more than what they have projected for each quality-adjusted life year.
Dr. Vincent Rajkumar – Now, the second question you said is, like, is there…, is this a good time or, you know, do we have enough data to answer these questions and there will never be a good time. We are having… We do have three new drugs approved in November. There…, there are, like I said, six active drugs that are going to come out very soon because we have six drugs at least that have single-agent activity, many in phase III trials and they will…, you will always be chasing the tail. So, insurance companies have to reimburse, provide right now to all patients who are around so there is…, there is no such thing as a good time, bad time. The data will continue to improve. I think this is the first report and hopefully as time goes on and more data comes in, this…, this will be continuously improved. There is… As Gary said, he is more concerned about ICER and patients than part B. They are all interlinked. Its just like one big circle of life. Its just all interlinked. I think the key to keep in mind is no one is against patients, not me, not ICER, not the doctors, not the insurance companies, not pharmaceutical companies. Everybody wants to do the right thing. What people want to do is avoid waste. If…, if…, if somebody is doing…, like tomorrow, if I decide by myself to give lenalidomide and ixazomib maintenance to all my patients, that just doubles the cost. Am I justified in doing that? Is that something that all other experts will agree on? Is that the best thing for patients? Is that shown by randomized trials? That’s the way to think about it, that people are trying to see, you know, what’s the best practices, rather than trying to restrict options. I…, I doubt we will ever in the US come to a situation where you as the patient I feel need daratumumab and…, and they won’t let me give it to you for some cost reason. That’s… I don’t…, I don’t see that happening. I don’t think you need to be worried about that. What could happen is if I want to use daratumumab as frontline, then somebody would say, well, listen this is approved in third line, not a single randomized trial has been done in frontline, maybe we shouldn’t give it or something, but I have not had this kind of thing happen and whether it be a PET CT or daratumumab or a new drug that’s going to come out, I fight tooth and nail with the insurance companies to make sure when I wear the doctor’s hat to get it for my patient.
Nick Van Dyk – Fair enough. I appreciate that. I am trying to not just ask the same question that everyone else has a different way. I have a second question which is sort of both individual and practical, but its really a theoretical question. You mentioned the cost, you know, let’s… I am sure it was a…, a straw man number for the sake of argument, but if it cost 200,000 dollars to treat in Minnesota, it costs a lot more than that in Arkansas and perhaps now in the upper east side of New York. I am joking because as you may recall from previous panels, I went through a regimen called total therapy which for those that are unaware of it, its an expensive protocol because it relies on an entire arsenal of drugs being used on a disease as frontline treatment and its maintenance regimen includes multiple years of Revlimid and other expensive drugs even in patients that don’t have any detectable disease; and normally on these panels, I am a pain in the ass about getting people to admit that it might be curative to some percentage of the patients, but let’s assume its 15% of patients, which is a low number by Bart’s estimate to be sure. If anybody is being cured, there is a first do-no-harm ethic here and…, which is ironic because that’s the key argument against total therapy or one of them, but if we look at what’s happened in the UK where I realize its certainly a different system, but, you know, let’s assume Bernie Sanders gets elected, we might be closer to nationalized healthcare than anybody currently thinks and if the UK now refuses Revlimid and pomalidomide for relapsed patients, its not that difficult to envision a scenario where something similar could happen here and you mentioned Abraxane for pancreatic cancer, that’s no longer allowed there as I understand it, neither is the breast cancer treatment. So, its not just myeloma. How under the first do-no-harm ethic can we be confident that the findings in this paper won’t work to undermine the availability of drug combinations or extended maintenance that could be curative if they are just deemed too expensive?
Dr. Vincent Rajkumar – So, again, Nick, I am not sure what actually happens with these. I can just go by what is available for me to review. I…, I don’t think that a non-profit organization has that kind of power that you think that they do like NICE does or the health authority in France or…, or the provincial authorities in Canada do; however, the principle is important. Number 1 is that no one will prevent you from getting like total therapy three types of experimental therapy. Remember, Bart did all of those on a clinical trial. He signed an informed consent and its a…, its a clinical trial. We are planning a clinical trial for high-risk smoldering myeloma that Dr. Kumar is doing as end-trial. If you think the current standard of care for smoldering myeloma is observation, what on earth are we doing with a trial where we are saying we are going to give carfilzomib-len-dex plus daratumumab for four cycles, then do a transplant, and then get more carfilzomib-daratumumab and then get maintenance for a year. I mean, how on earth can we possibly…
Dr. Vincent Rajkumar – No, that is a clinical trial and we are asking an experimental question and…, and we, you know, its very different scenario. In the…, in the UK, the reason that they are saying no to Revlimid or pomalidomide, I don’t know the details, but if they are saying no to some of these or to Abraxane, its not because they hate these drugs or they don’t want to help their patients. Its because there is only so much money and the only conclusion you can make is that the price charged by the drug companies is far too much for that economy to bear and…, and if the drug companies are walking away, it only means that that much profit is not meaningful to them because they can survive without it and…, and it also then means that they have another place where they can make that profit. No wonder all cancer drugs cost twice as much in the US and we have a table, I think, we…, I think Hagop has published a whole table of drug prices, how much they cost in other countries compared to the US. So, if we can negotiate just like NICE, we would be…, we would be able to lower prices.
Nick Van Dyke – Thank you.
Gary Petersen- Well, yeah, thanks, Nick. I appreciate that. We are running a little bit behind; and as a result, I am going to ask Yelak and Lori if they could just ask one question each to get us caught up and Yelak?
Yelak Biru – Sure. Dr. Rajkumar…
Gary Petersen- Sorry.
Yelak Biru – Thanks for… Yeah? Can you hear me?
Dr. Vincent Rajkumar – Yup.
Gary Petersen- Yes, yeah.
Yelak Biru – Okay. Thanks for putting yourself out there and advocating on behalf of all of us. I strongly believe that unless those that don’t directly benefit from change advocate for it, change won’t happen. In my mind, there is no question that drug prices are high, and they are the fastest growing component of our total healthcare expenditure. Do we need to discuss how to make this approved in available drugs and drugs that are also in the pipeline are readily available to patients? Absolutely, but in this case, I am reminded of the Star Trek analogy where all the data and all the logic is Kirk and not Spock, the Captain of the Starship USS Enterprise, right, which I think means data does not always translate to good judgment, especially in this case, the drugs just became available and I am not sure there is enough data to support some of the recommendations that are in the ICER report and specially for a disease like our’s where my treatment is different from Jack’s treatment and is different from Gary’s treatment, but I am not necessarily asking about that. I am asking about the unintended use of the ICER report such as you mentioned being able to hop the…, the freedom to do off-level prescription based on your judgment and your understanding of your patient. How do you prevent forced sequencing based on the cost rather than your understanding of me as…, as a patient, from Medicare or insurance companies putting some arbitrary sealings on that, but I think most importantly, quality in my opinion is defined individually. What is quality of life for me at a younger age than, say, Jack is different than Jack’s definition of quality of life and I am not sure how you are able to mathematically assess a quality life for me versus for some other patient and be able to take away that collaborative judgment that you and I are the doctor the patient can have. Can you try to bundle all this and try to answer them?
Dr. Vincent Rajkumar – (Laughter) Again, I think I…, I sense a lot of panic in many patients about whether the ICER report would mean that they will not be able to get the best treatment or whatever their doctor thinks is the best treatment, which could be completely off label, completely made up regimen and I doubt that that will happen. I want to keep on reassuring even though I am not part of ICER and I have no authority to say anything like that. I just don’t feel like that will happen in the US because we are able to talk to insurance companies and…, and they…, they could have denied me any number of times, but recently I published a case report of a patient where I just gave my 14th regimen, which had five drugs that have never ever been mixed together in a cocktail. They let us keep doing this because they are interested in the patient’s life and well being and, you know, we can always reasonably negotiate with them. I don’t think that this is…, think of this more as information that will help actually physicians make a good judgment. If…, if I knew ahead of time that it costs, I have…, I could reasonably choose these four regimens, but one costs one-fourth of the other and all of them are reasonably effective and you and I think that we should go for the, you know, the best one that’s also cost effective for you. Then, this gives me the information to make that pick.
Dr. Vincent Rajkumar – Rather than looking at this and saying that somebody is going to tell that he can only choose regimen A which is the cheapest and he cannot choose these other ones which I think is farfetched. I don’t think that’s the goal of…, of any of these, but its…, it does…, it is important for us to know what value is, that’s first. Secondly, you know, when you talk about quality of life and QALYs, I think I need to explain this because I saw even Gary tweet something which I wanted to…, to…, to clarify to him. You have to really understand QALYs well, like, for example, if I have a drug and I take it, I am a cancer patient and I live one extra year and the drug gives completely no side effects and I live one extra year just purely because I took that drug. That is called one quality-adjusted life here gained. That’s one QALY. However, if that drug was so horrible in side effects that six months of that year I am bedridden, I can’t even move, I am like in a coma and only six months I can actually live. Then, you don’t tell that that drug prolongs life by one year. You say it prolongs life by half a year. That is quality-adjusted life.
Dr. Vincent Rajkumar – This is very important because when…, when a company goes to countries like the UK or Canada or Europe, in…, in countries in Europe, they have to show what is the actual value provided by the drug and countries based on how much they can economically bear will say that for one extra year of life, this is how much maximum we can afford. Its not that they are bad intention, this is all their economy can support. So, in the UK, there is no fixed number. They are willing to work with companies, but in general, the UK would pay about 40,000 dollars per extra year of life. Europe maybe 60,000 dollars. Canada may be little bit more. We have drugs and regimens in the US that cost more than 250,000 dollars per quality-adjusted life year. That is jarring when you see it in the…, in the…, in the ICER report. It is jarring when you know that what is economically sustainable is usually two to three times per capita, meaning we should all be about 100,000 to 150,000 is what we could potentially afford and if you think of 250,000 per year and think that that doesn’t even factor in daratumumab, then you start to understand why we need some metrics because that…, then actually we can show to pharmaceutical companies and say that for the value your drug provides, you are pricing these drugs too high, rather than look at ICER and say like, how dare you issue a report which says these drugs are expensive. They didn’t set the price of the drug.
Gary Petersen- All right. Yelak, if we could move on then to Lori’s question…
Yelak Biru – Please.
Gary Petersen- …and, doctor, thank you. Do you mind if we take a few extra minutes here to…
Dr. Vincent Rajkumar – No problem.
Gary Petersen- You have a few extra minutes?
Dr. Vincent Rajkumar – Yeah, its fine.
Gary Petersen- I appreciate that. Thank you so much, doctor, and…, and thank you for all that you do. I am…, I am thankful and I pray that you never give up this fight. Lori!
Lori Puente – Thank you, Gary, and thank you, doctor. I want all my questions to be different now that I have listened to everything, but I am going to try to stick with the one that I have, but I…, I do want to make a statement that I have felt very strongly. We haven’t talked about very much how flawed this report is. We’re…, we’re focused on the cost of drugs. I think that’s a fair discussion. I don’t think its a fair discussion to talk about the cost of drugs just with multiple myeloma. That I think is very unfair because we are such a small population pool that has as yet no for-sure cure and so while Nick was on a clinical trial for total therapy, my husband was on total therapy, but he was not part of a clinical trial. That’s not the only way that we could get it and you have mentioned it was an elderly disease, I am…, I have very strong opinions about that. We met a 16-year-old patient in Arkansas. My husband was 48 years old. Most of the patients I know are not elderly. So, there is lots of frustrations that I have about why I chose an orphan disease that is suddenly experiencing some major research interests over the last 10 years, increased quality of life, not one year, but from one to three to five to…, you know, three to five, to five to seven, and in…, in the tenures that we have been dealing with this disease ourselves personally. So, there are lots of reasons to move forward and I am just very concerned about your not talking how this report presented multiple myeloma as a one-size-fits-all disease. Its not and you know that because you treat patients and you look at their genetics and you are looking at their age and you are looking at whether they have diabetes, heart disease, or whether they are 32-year-olds with small babies at home and have no other health issues. We are not a one-size-fits-all in treatment or how we present or age or anything. So, I would just like you to address your concerns about how flawed this report is in terms of its overall presentation, not just the cost of the drugs but how its presented our disease.
Dr. Vincent Rajkumar – So… Thanks. First of all, thanks, Lori, for…, for being there and for asking this question and I know we…, we have conversations on Twitter. You want to focus on the ICER report and…, and.., and go over that. Let me just tell you like, first of all, I…., I do know myeloma affects patients of all ages and its just that the median age is 65, that means half the patients are older than 65 and that means half the patients depend on Medicare for reimbursement of their drugs, like part B or part D and the more Medicare gets bankrupt, the more that is threatened and that’s threatened the more the price of the drugs. That’s the first thing to keep in mind. Younger patients with insurance are also at risk because many may not have good insurance that covers cancer chemotherapy and then many may have insurance but they have to pay 20% co-pay, which is extraordinarily expensive.
Lori Puente – Excuse me, one minute. You…, you say that a lot, but isn’t… Let me just clarify for my own because I know every insurance is a little different. When you say they have this 20% co-pay, my understanding is that 20% co-pay is up to whatever deductible they have chosen.
Dr. Vincent Rajkumar – Yes and some people have chosen..Lori Puente – Is that your understanding as well?
Dr. Vincent Rajkumar – Yeah, some people have chosen like that…
Lori Puente – Okay, so its not…, its not 20%…
Dr. Vincent Rajkumar – …and then they end up with this.
Lori Puente – Right, but its not 20% of the 200,000 dollar a year cost. I just want to get that straightened. Its 20% up to say 3,000, 5,000, whatever their annual deductible is. Is that your understanding as well?
Dr. Vincent Rajkumar – Yeah. It depends on the insurance premium, like the patient I saw who is actually willing to be interviewed by any news reporter, she was actually paying 4,000 per month and was in tears in my office. I don’t get into the details of patient’s insurance thing because, you know, at Mayo we are all salaried, we don’t get involved with this stuff, but at the same time I do see patients suffer and its something that we have to be aware of, that it doesn’t matter who is paying, someone is paying. If the drug costs 300, 400… If the regimen costs 300,000 dollars per year, that money is coming from someone’s premiums and someone’s co-pays but let’s not get into that. I mean your…, your question was on ICER and…, and…, and the thing is that I have also read the report and I think as I showed many of the other people before, I…, I am very puzzled about why everyone thinks that this will somehow limit their access to whatever drugs they need.
Lori Puente – No, my question was…, my question was how did…, how did you justify the…, the way the report is written as a clinical specialist with multiple myeloma where it has not presented us as the heterogeneous disease that we are, its presented us as a very homogeneous disease and that right after that…
Dr. Vincent Rajkumar – No. No, no, no.
Lori Puente – …made it difficult for me…
Dr. Vincent Rajkumar – Listen, again… You are…, you are talking about a report…. The…, the final report is after the committee has heard everybody. They are going to listen to me. They are going to talk about everything. This is just what they have assembled, then they have…., whatever they put out, but I know and they know that myeloma is not a homogeneous disease. Its seven different cytogenetic subtypes. Every patient responds differently. We choose drugs not just based on, you know, what the literature shows. In fact, many of the new regimens are not applicable to the patients in the US because most patients in these trials receive…, did not receive lenalidomide-dex, whereas most patients in the US would have already received… So, I don’t think that…
Lori Puente – So, you are comfortable with how the percentage… I mean forget the drug cost for just a minute because that’s a fair argument, I don’t disagree about the cost of drugs across many diseases, not just multiple myeloma. I just feel very personally attacked because for such a small group we don’t have a big voice and, you know, if you tried to do this with breast cancer, you would get a whole different…, I mean just look at the mammogram changes, everybody went crazy, you know, and they have…
Dr. Vincent Rajkumar – Is there any particular sentence that you think that they said that you are homogeneous population?
Lori Puente – Just the…, just the overall presentation and the lack of patient input and it has this one size fits all, the…, the way that it looked to me…
Dr. Vincent Rajkumar – No, no, you know, you love to blame the…
Lori Puente – …when I read the report that made it very…
Dr. Vincent Rajkumar – No, no, no. Think about this, Lori.
Lori Puente – But that made it very hard for me to…
Dr. Vincent Rajkumar – No, no. Think about this, Lori. All the trials we have done so far and this is why I have been calling for trials which are at individual cytogenetic abnormalities. They can only go after the literature there is. If you look at all the phase 3 trials and the big trials we have done, we’ve considered myeloma as a homogeneous disease. We just take anybody who has myeloma who has failed one prior therapy. We just… That’s all. We just lump everybody together. We report the response rates of everyone together. We report the benefits of survival and progression-free survival with everyone together. So, that’s all they can go by in preparing a report like this, but it doesn’t mean that they don’t understand that there are subtle differences between… There are many big differences between the various myeloma categories, the big categories and then subtle differences even within those categories, but that kind of data is just not there to tell like, you know, how would a 4;14 patient respond to elo-len-dex versus a 14;16 patient. Its… The fault will be on the investigators. If we had done trials just for 4;14 or just for 14;16 myeloma, then we could talk, but when all the trials and all the literature is treating myeloma as homogeneous, then that is…, that is how a review article will be written. I will assure you that, you know, we will as myeloma investigators change this very soon. I have been wanting to write a paper on myeloma which is not on myeloma but multiple myelomas and…, and basically write seven articles on each subtype of myeloma treating it as unique diseases because each one of them has to be treated differently, they present differently, they behave differently. Unfortunately, our trials are still done treating the disease as one.
Lori Puente – Okay.
Gary Petersen- Okay. Hey, thanks a lot, Lori. I really do appreciate that and doctor as well. I don’t know if you have any…, any time left at all, doctor, for…
Dr. Vincent Rajkumar – I am happy to take questions that were submitted if there are one or two.
Gary Petersen- Okay. All right. Let’s…, let’s do that. Priya, could you bring on some callers and…, and thank you, Lori. I appreciate that we just…, you know, I mean there was just so much great conversation and its tough to, you know, tough to bring anything to a close. Priya?
Priya Menon – Yeah. Thank you, Gary. Dr. Rajkumar, I think…., thank you for the extra time and for answering the panel so very patiently. We have received some more questions. I think, during the discussion, we have covered few. There is another one just come up. The listener is asking Dr. Rajkumar, how successful do you think advocate might be at the May 26 CEPAC meeting in convincing the ICER to listen to the advice of myeloma doctors regarding the use and cost effectiveness of myeloma drugs and revise their report accordingly?
Dr. Vincent Rajkumar – I think, you know, again I have… This is my first time I am, you know, I am going to a meeting like this and I…, my first passion is multiple myeloma and I have been over the last three or four years involved with the cost of cancer care. We will go there and see, but I think… Knowing the people in the organization, I think they are going to be very receptive to any kind of input, particularly patient input. This is a multi-step process and I think people are being…, are worried prematurely because the first step is…, if.., if I were to write a review article, I would first write the review article myself. I then send it for peer review and then change the report based on the peer review comments and then you get published and then you get opinions on that. This is the same way, its an iterative process. Its like, you know, they put out a document they got and put the revised it. Then, they go to a public hearing, get input. You can’t judge how the questions will be answered before they are answered and be worried. Of course, all of us want the best for our patients and I think a lot has to do with trust. For example, what Medicare wants to do, people think that, you know, they are somehow prejudiced but or like against patient’s no or against doctor’s no. I mean these are all well-meaning people who are faced with a very big dilemma and they have to find out some way to solve this and…, and they are trying their best and so, I would say keep an open mind.
Gary Petersen- You know, I think one of our fears is that, you know, we look at ICER and we see it as synonymous with NICE and…, and NICE is an allocator of resources and if ICER happens to be just a, you know, you can take a look at this report and it says, you know, these are the economic values of the various things and doctors and patients should take these into account, you know, it will give you four extra months. Do you want to go through this for the four extra months, type of thing? If its used in that regard then, patients aren’t that concerned; however, we look at it because its already being equated…, ICER is being equated to…, like NICE and as a result we see that NICE almost didn’t allow the use of Revlimid in…, in the UK until they decided that a patient with myeloma actually…, a quality-adjusted life year is actually 1.4 times that of a normal person. That increases by 0.4 just to get the thing approved, you know, not less but more and…, and they did, in fact, do that because there was an upheaval. You know, the people in the UK went nuts, you know, the myeloma people with that. So, that’s our fear. That’s my fear. You know, I want these things available for me, you know, but I also want to control costs and I just don’t understand why our government doesn’t take, you know, just like they did with the utilities, you know, do price reviews for different things if there is a monopoly, like a drug, so that they do price reviews, but that’s again, you know, my limited view.
Dr. Vincent Rajkumar – See, and I think you’re worried, but again if you look at myeloma, we have made dramatic advances. This is not lost on anyone. In fact, the type of improvements in progression-free survival we see in myeloma trials, this is dramatic compared to the type of improvements that they see in solid tumors and they get very, very expensive drugs approved. So, I don’t think you need to be worried. I mean compared to other cancers, our drugs give us so much more bang for the buck and…, and, you know, we’ve…, we’ve made great advances. The second point is whatever improvement that we have seen in the first trial is not the real improvement ultimately. Like Velcade, when it first came out, in the first apex trial, it prolonged progression-free survival only by like three months or four months, but we all know now that Velcade alone probably added a year or more to patients’ lifespans. So, subsequent studies usually show much as we learn to use these drugs, much more benefit than they have and finally, you know, I really, as I told many, many times, I do not blame pharmaceutical companies. I think we… I have worked with almost all of them closely. I have led trials with pretty much all these companies. Without them, we couldn’t have done much of the progress in myeloma and its the system, its a system. When they are set up in a system where they can actually increase price and there is really no barrier to that and the buyer does not have to negotiate with them. If they choose to increase the price of a drug from 100 to 120,000 next year and the buyer just has to accept it and there is no law or anything preventing them from doing that, that’s the system that we have to change because that’s a temptation that I cannot ignore if I were selling something.
Gary Petersen- You know, that’s why we have anti-trust laws.
Priya Menon – Thank you, Gary. Thank you, Rajkumar…, Dr. Rajkumar. I think I may go off in…, off air in 5 minutes. So, thank you, everyone, Gary, Jack, Cindy, Nick, Yelak, and Lori. Your support is always very encouraging and I hope…, and Dr. Rajkumar, you have reassured everyone here. I hope people now understand what’s happening and I hope something good comes out of the meeting finally in favor of the patient, of course. So, today’s talk will be made available on CureTalks’ website along with its transcript; and we are talking to Dr. William Matsui on 31st of May at 5 p.m. eastern on preventing relapse in myeloma. So, please do join us again and visit curetalks.com. Thank you.
Dr. Vincent Rajkumar – Thank you.
Gary Petersen- Thank you, Dr. Rajkumar. You are exceptional and thanks for everything you do for us. We thank you for that. Thank you.
Dr. Vincent Rajkumar – And thanks again for everyone for having me. Thank you.